The intensive care unit is not the best place for all Covid-19 patientsMoral outrage about limiting medical treatment in some coronavirus cases is misplacedDavid Oliver April 18 2020
The writer is an NHS consultant physician, a former vice-president of the UK Royal College of Physicians, and national clinical director for Older People’s Services 2009-13.The UK’s experience of the Covid-19 pandemic has thrown up some controversial stories about the
limits of medical treatment for infected patients who become dangerously unwell.
But doctors have been discussing death and dying with patients and families long before this crisis — and finding out their own goals and wishes. We have not just reinvented advance care plans for those who may not be capable of making decisions later on. Nor is
palliative care to help people die with dignity and comfort a new invention for the coronavirus era.
National Health Service clinicians have documented “Do Not Attempt Resuscitation” (DNACPR) decisions and “treatment escalation plans” (about the level of intervention we provide for people at high risk of deterioration, as described in the NHS End of Life Care strategy in 2010) for years. There have also been for several years Early Warning Scores and there is now a
National Early Warning Score to spot signs of deterioration.
We have always had to choose carefully which patients are most likely to benefit from a spell on an intensive care unit, with or without intubation and mechanical ventilation. None of this is new. Yet it is only now generating moral outrage.
In actions widely reported a few days ago, it was considered insensitive that a GP surgery in South Wales wrote
letters to patients in high-risk groups urging them to consider DNACPR and “don’t convey to hospital” instructions. It was seen as equally ham-fisted for the Brighton and Hove Clinical Commissioning group to have written to
local care homes suggesting all residents should be put in those categories.
But let’s distinguish poor choice of language and a depersonalising style of communication from the general principles. For many years there has been a need for us to have more advanced care plans for people living with life-limiting, long-term conditions or age-related frailty. And when people do pitch up in acute hospital care without such plans, we also need to have more and better discussions at that point. These changes would help people who are dying to have more choice, control and better symptom relief when the time comes. Their families would also have a better experience of bereavement.
Forms such as Respect (
Recommended Summary Plan for Emergency Care and Treatment), introduced four years ago, are now widely in use, allowing us to go beyond a “yes/no” decision on resuscitation if your heart stops: it encourages us to consider quality of life in recovery versus burden of the treatment.
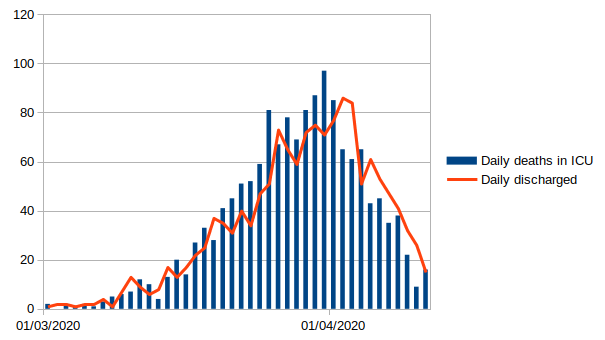
Admission to the ICU is no guarantee of recovery for many patients, nor is ventilation. Many will not survive or will live with long-term effects. The experience can be very distressing, and can include sometimes terrifying delirium. Even so-called non-invasive ventilation such as continuous positive airway pressure (which is used as a step before intensive care for people with respiratory distress) can be claustrophobic and frightening, especially for frail or confused older people. The processes can also be disturbing for their families. So this is not a black and white case of “intensive treatment good; supportive care bad”.
Even for patients in hospital, cardiopulmonary resuscitation does not have anywhere near the survival rate depicted in popular medical television shows; in many cases, performing CPR amounts to a ritualistic and undignified medicalisation of natural death.
Good palliative care to relieve distress and provide dignity would often be better. Care home residents are often in poor health and often in their last year or two: 59 per cent are aged 85 or older,
according to the ONS. They rarely do well if they undergo CPR, and conveyance to a busy, noisy acute hospital can be distressing and often leave them dying away from familiar surroundings and faces.
People with dementia, with learning or physical disabilities, or groups advocating for them, have raised understandable concerns that medics will somehow make “quality of life” assumptions or decisions and deny them treatment from which they might benefit. I realise that medicine has at times let such citizens down or discriminated against them, but I see no evidence or prospect of this approach being taken during the pandemic.
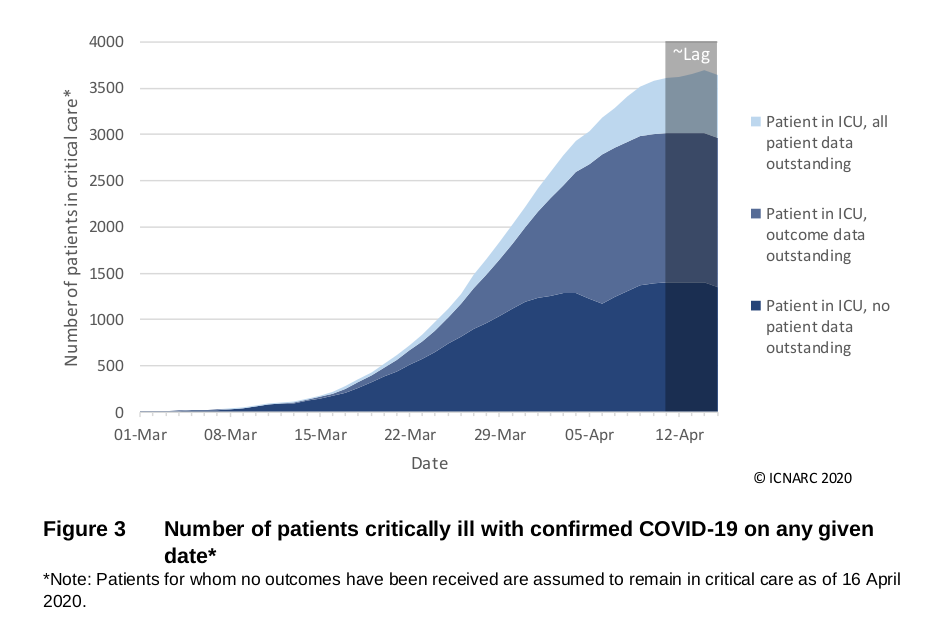
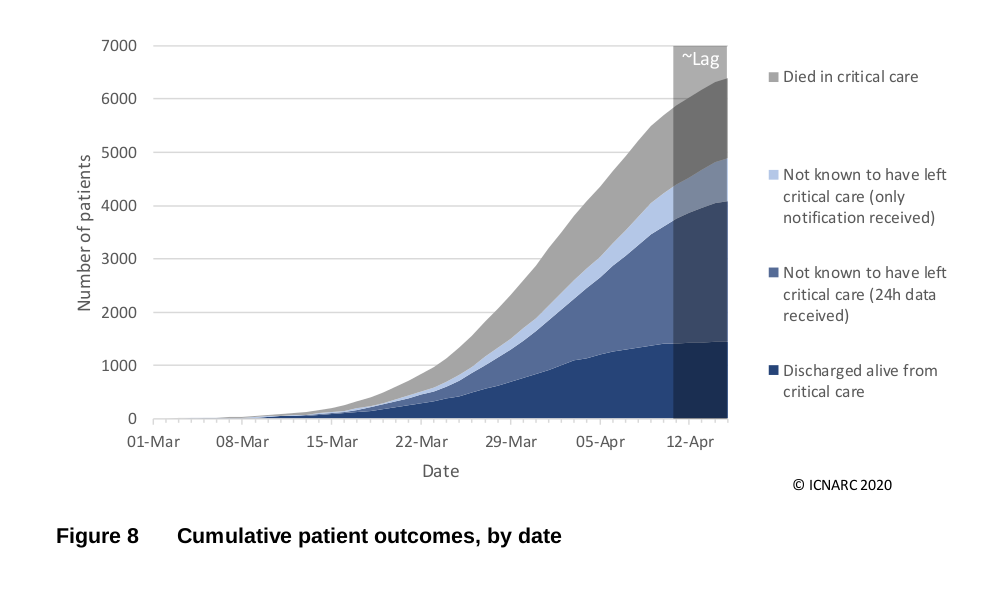
If we really do hit a peak of demand that overwhelms our much-expanded intensive care capacity, there may in extreme cases be hard choices to make between
two patients who could both benefit from admission. We aren’t quite there yet. Open decisions and discussions about limits of treatment are what we should have been doing all along. We are now merely talking about them openly.
Once the pandemic is over, let’s hope this is our new, demystified normal.